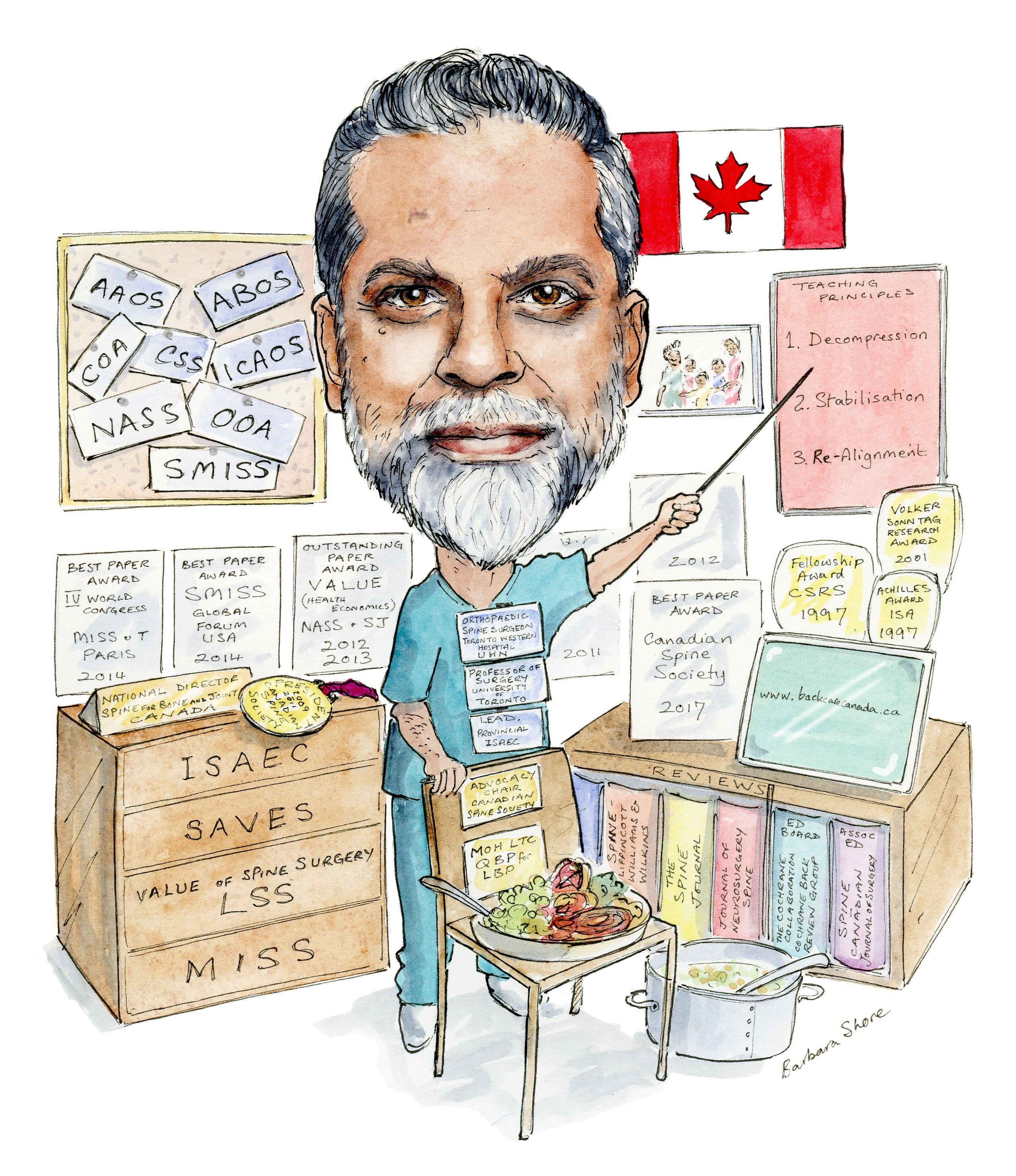
An advocate for interprofessional models of care for spine and musculoskeletal disorders, Raja Rampersaud is a spine surgeon globally recognised as a leader and innovator in the minimally invasive field. His clinical research focuses on health services and quality of care, including comparative/cost-effectiveness analyses for orthopaedic disorders such as low back pain and osteoarthritis. He speaks to Spinal News International about his proudest career achievement, the Canadian healthcare system, and his passion for cooking.
When did you know you wanted to go into medicine, and what drew you to spine surgery specifically?
I always thought I was going to be an engineer, but was intrigued with the mechanics and complexity of the body, so Orthopaedic surgery presented itself as the best of both worlds. As a resident in orthopaedics, I initially wanted to do sports medicine, but after my first exposure to anterior spine surgery (it was a thoracotomy approach for a metastatic spine lesion causing cord compression), I was hooked. I found dealing with the anatomical complexity (including adjacent visceral and vascular structures), mechanics and the delicacy of neural structures of the spine intriguing.
Have you had important mentors throughout your career? What have they taught you?
I have had many mentors over the past 30 years, but four have provided me with the skill set that drives much of what I do today. Kevin Foley, who during my fellowship taught me the importance of being meticulous from both a clinical and academic perspective. Robert Bell, former CEO of my institution and now Deputy Minister of Health for Ontario, for broadening my perspective and approach to clinical care and research. Nizar Mahomed, my colleague, who has taught me that leadership is about elevating the collective, not the individual. Hamilton Hall, for showing me that being a surgeon is so much more than performing an operation.
What is your proudest career achievement to date and why?
In 2007, I decided to do something proactive about my long waiting list and inefficiencies of our otherwise amazing universal health care system. I started work on assessing and improving care for spinal patients and laying the necessary ground work for alternate models of care for patients requiring assessment and management of spinal symptoms. As an elective condition, it could take upward of a year before someone saw the right specialist provider.
My work has led to my current recognition as the clinical lead for the Ontario Ministry of Health and Long-Term Care (MOHLTC) LBP [lower back pain] model of care initiative. I led the development and implementation of the MOHLTC Inter-Professional Spine Assessment and Education Clinic (ISAEC: www.ISAEC.org ) pilot project.
To date the ISAEC pilot has cared for over 6,500 LBP patients and has been effective regarding patient access to secondary and tertiary assessments (<2-6 weeks), patient satisfaction (consistently >95%) and improvement in validated patient reported outcomes. Our network providers (primary care doctors, nurse practitioners, chiropractors and physiotherapists) consistently report a high satisfaction rate (97%) with 96% noting that the ISAEC- model has improved their ability and the overall care of LBP patients.
The educational resource and the shared care aspect of the ISAEC-model of care essentially provide continuous education and knowledge translation activities (including monthly inter-professional news-letters and case conferences). Additionally, our networked spine surgeons report high appropriateness of referral and change in their practice profile, wherein high risk patients that could benefit from time sensitive specialised interventions are being referred dramatically earlier.
From a system perspective, ISAEC has shown efficiency, with network specialists no longer using advance imaging to screen referrals that come from ISAEC providers, and from a broader system perspective, the ISAEC networked primary care providers have demonstrated a greater than 30% sustainable reduction in spine imaging in the first two years of the ISAEC programme. ISEAC is currently being rolled out as a full scale provincial program over the next two years (2018–2020) and will serve over 10 million adult Ontarians.
How has the field changed since you started your career?
There is a welcomed and desperately needed focus on determining and improving patient outcomes in an evidence informed, systematic manner. While surgical innovation requires anecdotal expertise (and I have provided my fair share), not everything in—in fact the majority of—surgery is amenable to an unbiased RCT [randomised controlled trial]. We are seeing the power of prospective registries to provide real-world data on the outcome and value of spinal surgery for common condition.
Outside of your own research, what is been the most interesting paper that you have seen in the last 12 months?
The recent paper by Khor et al (Khor S, Lavallee D, Cizik AM, Bellabarba C, Chapman JR, Howe CR, Lu D, Mohit AA, Oskouian RJ, Roh JR, Shonnard N, Dagal A, Flum DR. Development and Validation of a Prediction Model for Pain and Functional Outcomes After Lumbar Spine Surgery. JAMA Surg. 2018 Mar 7). Consistent with our current work, the use of prognostic factors and real-time predictive analytics have the potential to be transformational in shared patient decision making and improving the outcomes of surgery.
In your opinion, what are the most exciting new developments in spinal surgery that we can expect in the next five to ten years?
As per the article noted above, the use of predictive analytics and big data from registries with adequate granularity (i.e. clinical and patient reported data beyond that which exist in legacy administrative datasets) will be critical to achieve the triple aim of value-based care. This applies to many aspects of healthcare and in particular subspecialised care.

What is the biggest challenge in spinal surgery at the moment?
Keeping up with the pace of technological and surgical technical advancement, and demonstrating their value from a patient, societal and payer perspective.
A lot of your research focuses on the cost-effectiveness of orthopaedics—when did you become interested in healthcare economics, and why do you think it is an important topic for surgeons?
At the start of my career as a consultant spine surgeon, I noted my patients where very happy with the outcome of their surgery, and could not reconcile the general perception of some of my non-spine colleagues who felt that the outcome of spinal surgery was questionable. If that was the case, then why the heck am I a spine surgeon? This led me to reflect on the fact that the broader perception of spinal surgery (the public, non-spine surgeons, payers, and the media) was even worse. In challenging economic times, the maths is pretty simple: if you cannot prove your value, you are NOT going to make the ‘cut’.
Could you explain your current research interests?
My research interests are focused on prognostic research and medicine for degenerative lumbar spinal disorders and determining parallels that exist with osteoarthritis. This focuses on determination of prognostic factors for operative and non-operative interventions, comparative/ cost-effectiveness studies and integration of prognostic medicine into musculoskeletal models of care that improve the care quality, outcome, and cost (i.e. the ‘triple aim’).
As a surgeon in Canada, how does the Canadian healthcare system help and hinder your research and/ or practice?
Our Canadian Healthcare system offers universal access and a high-level of care for all; however, non-emergent or urgent musculoskeletal conditions are associated with long wait times for specialist assessment and surgical care. This represents a significant barrier that inspires care innovation by often doing more with less. The nature of our system allows for assessment of the natural history of the condition and provides reliable long term follow-up. As a surgeon, admittedly, our cost limitations do create a degree of frustration in the ability to bring new technologies to patients in a timely manner.
You are an advocate for interprofessional models of care for spine and musculoskeletal disorders. Why is this important to you?
I strongly believe, no one provider can effectively provide all the needs of a spine patient (or patients with other chronic conditions). Integrated, interprofessional models of care using patient centred, shared care principles provide more consistent and better-quality care while reducing the mixed patient messaging and care fragmentation that occurs in most current healthcare delivery systems.
As the current Advocacy Chair for the Canadian Spine Society (CSS): what does this role entail? What are the biggest advocacy challenges facing the spinal field?
At the present time, along with the rest of the CSS executive, this role entails engaging our membership in research through the Canadian Spine Outcomes and Research Network (CSORN) that is focused on showing the ability of spinal surgery to positively impact a patient’s quality of life, provide societal benefits at a national level, and enable national data generation regarding the negative impact of patients on prolonged wait-list for elective surgery. In-order to maintain, and where possible increase, surgical spinal care funding, this type of information is essential for surgeons to advocate at local and provincial levels.
What is a highlight of your time as president of the Canadian Spine Society?
Developing advocacy efforts to challenge the public and professional misconceptions of spinal surgery. Specifically focusing on the fact that many view spine surgeries as costly and ineffective and tend to lump everything we do as dealing with ‘non-specific back pain’. Non-specific back pain is principally a non-surgical issue, and depending on the type of practice and where you are around the world, only represents a very small, sometimes non-existent, proportion of what spine surgeon operate for. In appropriately selected patients with diagnoses such as neurogenic claudication due to spinal stenosis, we provide the same degree of value to patients and payers as does total joint replacement.
What advice would you give to someone wishing to start their career in spinal surgery?
The opportunities are tremendous. Open your eyes and ears, and do not be afraid to think big!
What are your interests and hobbies outside spine?
My wife Samina and I have four children (Amira, Sofia, Isa, Aliya) ages five to 12 that keep us extremely busy! We love to cook, travel, and watch movies. At least once a week, I enjoy making a gourmet meal for my family and as often as possible for guests. I find cooking creative, relaxing and a wonderful bonding experience.
Fact file
Current roles
- Professor, Surgery, University of Toronto, Toronto, Canada
- Consulting staff, Division of Orthopaedic Surgery and Neurosurgery, Toronto Western Hospital, University Health Network, Toronto, Canada
- Advocacy Chair, Canadian Spine Society, Canada
Education
1998: Neurosurgical Spine Fellowship, Semmes-Murphey Clinic, University of Tennessee, Memphis, USA; Supervisor: K T Foley
1997: Orthopaedic Spine Fellowship, Victoria Hospital, Western University, London, Canada
1993–97: Orthopaedic Surgery Residency, Western University, London, Canada
1992–93: Rotating internship, St. Michael’s Hospital, Toronto, Canada
1988–92: Medical Doctorate, with Honours, Faculty of Medicine, Western University, London, Canada
Society roles
2013–17: Director, Spine, Bone and Joint Canada, Toronto, Canada
2013–15: Chair, Minimally Invasive Procedure Sub-Section, USA
2009–11: President, Canadian Spine Society, Canada
2007–08: Chief of Trauma Section, Orthopaedic Oral Examination Committee, Royal College of Physicians and Surgeons of Canada, Canada
Awards (selected)
2017: Best Paper Award, Canadian Spine Society, Canada
2014: Best Paper Award, Principal Investigator, IVth World Congress of Minimally Invasive Spine Surgery and Technqiues, Paris, France
2014: Best Paper Award: 2014 Annual Meeting, Principal Investigator, Society for Minimally Invasive Spine Surgery-Global Forum, USA
2013: Outstanding Paper Award: Value (Health Economics), Principal Investigator, North American Spine Society and The Spine Journal, USA.
2011: Outstanding Paper Award, Value (Health Economics), principal investigator, North American Spine Society and The Spine Journal, USA













I would love to get Dr. Rampersaud’s opinion on the option of back surgey in my case vs. doing nothing other than maintenance with chiropractic, core exercises etc. Don’t know if he at all takes personal requests. I am not a patient of hi. I am in Ottawa and seriously toying with the idea of surgery. Have done a year of Neurostructural Correction with a Chiro, not sure if that is the longterm answer. Is it possible to send him copies of my x-rays and MRI or can he recommend a surgeon in Ottawa.
Any help appreciated.