
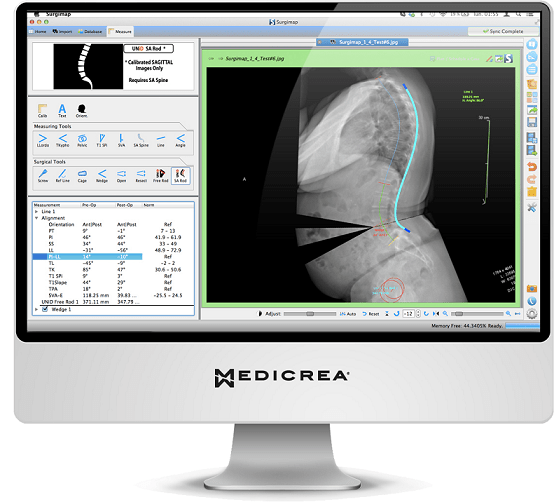
The use of computers to map the spine, to plan surgery, and to aid in the manufacturing of medical devices is becoming increasingly common in spinal surgery. Spinal News International speaks with Andrew G King about his experience with patient-specific rods (UNiD, Medicrea), designed using preoperative images and spine-specific planning software (Surgimap).
Which patients do you think could benefit from surgical approaches to scoliosis?
Surgery is recommended in those people whose spinal curve has progressed to a certain level of severity, particularly where there is documentation of progression despite all conservative treatments. While progression is most rapid during the preadolescent growth spurt, there is a certain level of severity where scoliosis is known to increase despite the end of growth.
In addition to curve severity, I am more inclined to perform surgery if the patient has a major concern about the effect of scoliosis on appearance—especially a very obvious hip offset or large rib prominence. The presence of pain or fatigue associated with the scoliosis may also be weighted into the decision.
What do you see as the biggest barriers to successful surgical scoliosis treatment?
In the past, the measure of a successful surgery was solely related to the percentage of correction on the coronal X-ray. This has radically changed over the last decade with the introduction of quality of life metrics such as Scoliosis Research Society-22 questionnaire and calculation of Quality-Adjusted Life Years.
There is increasing evidence that harmonious sagittal balance is more important than the percentage of coronal correction in achieving a satisfactory result and a successful outcome according to these measures.
How important is sagittal balance in adolescent idiopathic scoliosis treatment?
In adolescent idiopathic scoliosis, the sagittal malalignment is more subtle than in cases of adult degenerative scoliosis. We believe, however, that it is equally critical in the long term. We expect that most of these patients will have to live with their sagittal profile for over 50 years! It is interesting that adults with untreated adolescent idiopathic scoliosis commonly complain of fatigue, which may be caused by sagittal malalignment.
What other benefits have you experienced using a patient-specific rod system?
There is the obvious benefit of saving operative time spent manually bending rods. We have documented that this translates into shorter total operative time and less blood loss. We are currently looking at our patients to see if we can quantify improved sagittal parameters that we believe will translate into improved postoperative quality of life measures.
It is our impression that we have seen an improvement in thoracic hypokyphosis. Increasing the thoracic kyphosis often translates into improved cervical and lumbar lordosis and a more normally aligned sagittal vertical axis. An early observation is that our manually bent rods had been incorporating too much lumbar lordosis, resulting in a negative sagittal vertical axis. A negative vertical axis has recently been shown to be a cause of proximal junctional kyphosis.
There is a wide variety of values of pelvic incidence, lumbar lordosis, and thoracic kyphosis from one individual to another. Early in the use of patient-specific rods, I first “eyeballed” a rod with a French bender to a configuration that I had been using in previous years. I then compared this bend to the patient-specific rod and was surprised by the difference.
Most commonly, I had been incorporating too much lordosis into the lumbar spine and starting the transition from thoracic kyphosis to lumbar lordosis too proximally, namely around L1 or L2. My faith in the patient-specific rod has been borne out of postoperative X-rays, which are showing a more normal sagittal balance than I had been achieving with rods bent by “eyeballing” and the use of a French Bender.
How easy is it to translate a software-estimated rod into actual spinal correction?
Our initial evaluation of our results with patient-specific rods has allowed us to be confident in incorporating them without any oversight or modification. Early on, we thought we observed some slight flattening of the concave rod during the correction process and suggested an extra five degrees of kyphosis be incorporated into this rod. This may or may not be necessary.
Does a patient-specific system have any drawbacks?
The software is utilised on a standing lateral scoliosis X-ray. After digitising the spine and carrying out the virtual corrections, the software outlines the rod dimensions which will be sent to the manufacturer. It is essential that the X-ray be taken with a calibration marker to prevent magnification. Currently, calibration markers consist of a metallic ball which the patient wears around their neck at the time the X-ray is taken. Early on, we did not have these calibration markers at peripheral clinics where radiographs were taken and the decision for surgery had been made.
The result was that the rods were routinely coming to us too long. This required cutting the rods down to size. With routine use of calibration markers, this no longer presents a problem and the rods routinely come close to the exact dimensions for each patient.
How expensive is this kind of a rod, as compared to a French Bender? Is this high-tech bespoke system accessible to smaller and mid-size institutions?
Most hospitals and institutions throughout the world, small or large, are increasingly being held to financial scrutiny of new products. Our institution is no exception. The technology was passed by the Finance Committee and we were surprised that it was approved. There may be additional savings in the reduced operative time and reduced blood loss.
In the long term, there may also be savings in that the improved sagittal balance may show a decreased need for reoperation, either for proximal junctional kyphosis, pseudarthrosis, or other problems.
What feedback have you received from patients who have undergone patient-specific treatment?
Patient feedback has been extremely positive, but cynics would say—quite justifiably—that nearly all patients with adolescent idiopathic scoliosis should do well in the first year or two following surgery. In our first 50 cases, there have been no revisions. The only extra surgery was in one case where a girl had her wound explored for possible acute infection a week later.
We plan to prospectively follow our patients with radiographs and quality of life outcome instruments at two and five years after surgery.
Andrew G King is an orthopaedic spinal surgeon at the Children’s Hospital, New Orleans, USA













