This advertorial is sponsored by Spine Innovations
 The ability to restore spinal function is an important consideration when choosing options for the replacement of degenerated discs in the cervical or lumbar spine—in particular when there is an alternative to spinal fusion, which can come at a cost of motion to the patient. Developed by FH Orthopedics and now marketed by Spine Innovations, ESP disc replacements use a patented viscoelastic technology to mimic the characteristics of and provide similar motion properties to a natural disc.
The ability to restore spinal function is an important consideration when choosing options for the replacement of degenerated discs in the cervical or lumbar spine—in particular when there is an alternative to spinal fusion, which can come at a cost of motion to the patient. Developed by FH Orthopedics and now marketed by Spine Innovations, ESP disc replacements use a patented viscoelastic technology to mimic the characteristics of and provide similar motion properties to a natural disc.
The technology has been widely applied and studied since 2004, gaining CE mark approval via the LP-ESP lumbar disc replacement prosthesis in 2006, and the CP-ESP cervical disc replacement prosthesis in 2012. The innovation began with the work of Raymond Roy Camille (La Pitié Salpêtrière University Hospital, Paris, France), who after inventing a pedicle screw that became the gold standard for spine fusions, assessed natural disc properties and designed a prosthesis to restore natural function.
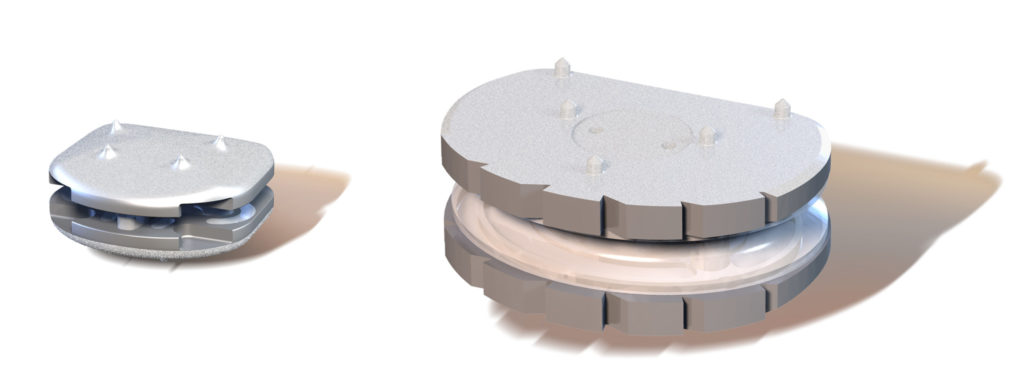
The LP-ESP and CP-ESP discs—the technologies that have resulted from Roy Camille’s work—are considered third-generation products in the development of total disc replacements. These are standalone prostheses, designed with an aim of facilitating osseointegration and improving the anchoring quality of the device. These aims are met in two ways. Firstly, the ESP prosthesis is made of two titanium alloy endplates and an elastomeric cushion. The spikes on the endplates outer surfaces improve primary fixation. And, perhaps more crucially, the titanium is coated with a second layer of hydroxyapatite (HA), applied using a plasma spray technology. HA is a completely inert mineral material and has been frequently used as a biomaterial in orthopaedics for cementless implants for several decades. Its composition is close to that of bone, giving it the potential to accelerate bone growth onto the implant.
According to orthopaedic surgeon and expert in bone substitutes and biomaterials Claude Schwartz (Clinique des trois Frontières de Saint-Louis, Saint-Louis, France), if the disc prosthesis is properly positioned, with good primary stability, and is not subjected to shear forces at the HA-bone interface, the time that the disc prosthesis is attached to the vertebral body should not exceed three weeks.
For Jean-Alain Epinette, an orthopaedic surgeon at the Orthopaedic Research & Imaging Center in Arthroplasty (CRDA, Bruay Labuissière, France), safety is an important aspect of the use of HA-coated prostheses. Epinette has studied the use of the material widely, in particular as means for long-term fixation of components in hip arthroplasty. “Two decades of hydroxyapatite coatings have also demonstrated that no real and effective adverse effects have ever been experienced with HA-coated implants,” he says.
Among Epinette’s work to validate the use of the material is a paper published in Hip International in 2008, in which he detailed over 20 years of experience with HA as an alternative to the plain porous fixation system used in hip replacement. Here he reported that HA in an “uncemented” fixation can be considered reliable and efficient.
“Calcium phosphate ions participate in the physiological turn-over of bone remodelling, and over years, the HA coating is replaced by new bone formation, without any fibrous tissue layer, even in difficult cases of gaps or immediate full-weight bearing. These HA particles are biodegradable and have never produced any inflammatory reaction in the surrounding bone. Fear of osteolysis or third body wear due to HA debris has never been confirmed by serious studies, conversely to PE [polyethylene], metallic or cement particles,” Epinette says.
“I have used HA-coated implants for hip and knee implants for up to 30 years,” adds Jean-Yves Lazennec (Department of Orthopaedic and Trauma Surgery, La Pitié Salpêtrière Hospital, Paris, France) on the properties of the HA coating and its performance in patients. He comments: “In my experience, it significantly favours bone growth at the interface between the implant and the bone. My feedback is the same for disc replacements, having used them for 15 years.”
Lazennec is among those to have studied the use of the ESP disc replacement most widely, authoring numerous papers to examine the prosthesis spanning several decades. Writing in the European Journal of Orthopaedic Surgery & Traumatology, Lazennec documents clinical experience of the CP-ESP cervical disc prosthesis, noting that two-year follow-up data for the device are “encouraging for pain, function, and kinematic behaviour. “The prosthesis geometry allows limited rotation and translation with resistance to motion aimed at overload of the posterior facets,” Lazennec writes. In a further clinical study in The Spine Journal, he also details the clinical outcomes, radiologic kinematics, and effects on sagittal balance of the LP-ESP disc prosthesis. Here, he reports that the prosthesis recreates lumbar function similar to that of a healthy disc.














Is it possible for cervical or lumbar artificial discs to pop out of place? Are they held in place by some method i haven’t seen in simulations of the procedure?